Preauthorization
Before you can schedule certain healthcare services you may need to get preapproval from your insurance company. This is called preauthorization. (The terms precertification, prior authorization, and prior approval are also used, and they all basically mean the same thing.) For example, services that may require pre-certification include outpatient and inpatient hospital services, observation services, invasive procedures, CT, MRI and PET scans, and colonoscopies.
In the medical billing world, preauthorization, prior authorization, precertification, and notification are terms that may be used interchangeably to mean that for certain situations and procedures, providers have to contact insurers in advance and obtain a certification number in order to be reimbursed properly (or at all) for services. Insurance verification and insurance authorization services play a vital role in revenue cycle management. In fact, most claim denials happen when a patient is ineligible for services billed by the provider.
If an authorization is required you can usually obtain it from the insurance company over the phone. Some companies have special forms that they want faxed in to them. Usually they will issue you a number or a series of numbers and letters which you will enter on the insurance
claim in box 23. Authorizations are usually given for a certain number of visits over a certain period of time.
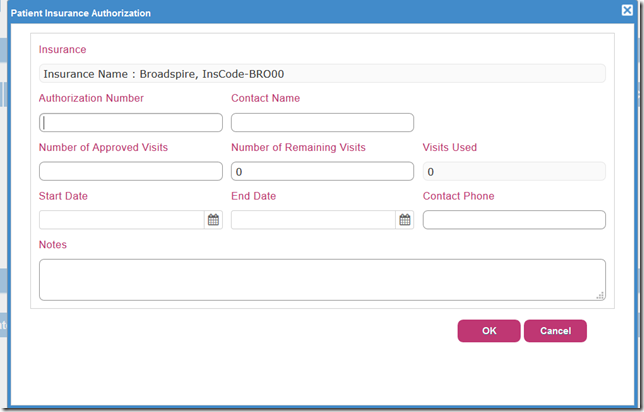
Typical Screen in PMS Software to store Pre Authorization Numbers by Payer.